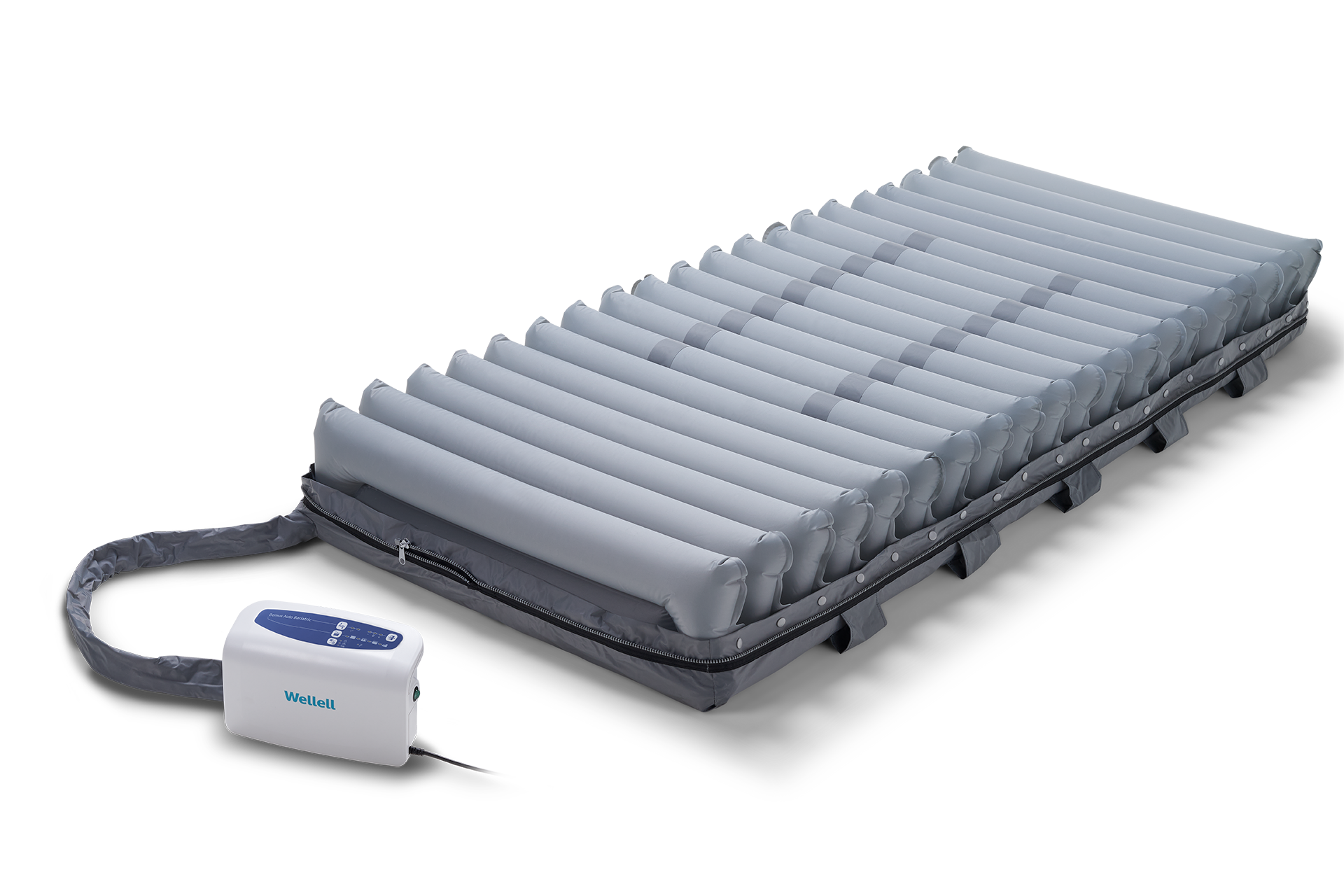
Domus Auto Bariatric
For Moderate to High Risk
Auto-adjusting pressure redistribution system — implementing early pressure injury prevention for long-term care bariatric patients
Obesity contributes to 26% of long-term care pressure injuries. Typically, bariatric residents are younger, healthier, and more independent, lengthening overall care stay and pressure injury treatment.1-2
Severely lacking of supportive equipment and resources inhibits bariatric pressure injury prevention, significantly increasing nursing labor, time and health risks. 3-4
Domus Auto Bariatric’s wider surface automates firmness calibration and provides sacral pressure relief, ensuring pressure relief, safety, and comfort in any position while minimizing caregivers’ labor.

Wider surface, auto-adjusting firmness
- Suitable for improving pressure injuries in long-term care and homecare bariatric residents.
- Wider surface with automatic firmness adjustment based on residents' weight distribution for quick setup and pressure relief delivery.
- Max firm function provides a static surface for nursing procedures.
- Provide effective pressure relief care with alternating pressure redistribution and constant low pressure modes.
- Heel relief function provides easily remove the individual air-cell which can float the heels with zero pressure to prevent injuries on the heels.
- Visual and audible alarm enhances patient safety and security.
- CPR knob allows caregivers to rapidly deflate the mattress for emergencies.

Automatically adjusts to the most optimal pressure for the patient, ensuring both clinical effectiveness and cost efficiency.

Tuning function improve patient comfort by manually micro-adjust mattress firmness.

Seat inflation mode adjusts the pressure of the air cells, helping prevent bottoming out while sitting, thereby improving stability and comfort.

Specialized bariatric beds — wider — improve care quality and experience, minimizing nursing injury risks.
| Domus Auto Bariatric | ||
|---|---|---|
| Mattress Dimension (L x W x H ) | 78.7 x 41.3-47.2 x 8 in | 2000 x 1050-1200 x 203 mm |
| Mattress Weight | 15.2 lb | 6.9 kg |
| Maximum Patient Weight | 770 lb | 350 kg |
| Pump Dimension (L x W x H ) | 11.4 x 7.3 x 5 in | 290 x 185 x 126 mm |
| Supply Voltage | 220-240 V / 50 Hz |
|

Wider surface, auto-adjusting firmness
- Suitable for improving pressure injuries in long-term care and homecare bariatric residents.
- Wider surface with automatic firmness adjustment based on residents' weight distribution for quick setup and pressure relief delivery.
- Max firm function provides a static surface for nursing procedures.
- Provide effective pressure relief care with alternating pressure redistribution and constant low pressure modes.
- Heel relief function provides easily remove the individual air-cell which can float the heels with zero pressure to prevent injuries on the heels.
- Visual and audible alarm enhances patient safety and security.
- CPR knob allows caregivers to rapidly deflate the mattress for emergencies.

Automatically adjusts to the most optimal pressure for the patient, ensuring both clinical effectiveness and cost efficiency.

Tuning function improve patient comfort by manually micro-adjust mattress firmness.

Seat inflation mode adjusts the pressure of the air cells, helping prevent bottoming out while sitting, thereby improving stability and comfort.

Specialized bariatric beds — wider — improve care quality and experience, minimizing nursing injury risks.
All air cells are made from Thermoplastic Polyurethanes (TPU). It is highly resistant to breaking down when in contact with water (hydrolysis), soft to touch, and minimizes friction and noise during patient movements.
The cover is made with nylon/PU and is vapor permeable, fire-resistant, and water-resistant. See specifications for more details on the fire-retardant standards.
- Hahnel, E., Lichterfeld, A., Blume-Peytavi, U., & Kottner, J. (2017). The epidemiology of skin conditions in the aged: A systematic review. Journal of tissue viability, 26(1), 20–28. https://doi.org/10.1016/j.jtv.2016.04.001
- Dinerstein, C. (2022, August 24). Pressure Ulcers and Nursing Home Ratings. American Council on Science and Health. Retrieved May 11, 2023, from https://www.acsh.org/news/2022/08/24/pressure-ulcers-and-nursing-home-ratings-16508
- Lee, A. M., Sénéchal, M., Hrubeniuk, T. J., & Bouchard, D. R. (2020). Is sitting time leading to mobility decline in long-term care residents?. Aging clinical and experimental research, 32(1), 183–186. https://doi.org/10.1007/s40520-019-01148-z
- Park-Lee, E., & Caffrey, C. (2009). Pressure ulcers among nursing home residents: United States, 2004. NCHS data brief, (14), 1–8.